Gdm ncp
In true GDM, glucose gdm ncp returns to normal by six weeks postpartumalthough women with GDM have an increased risk of developing type 2 diabetes mellitus later in life, gdm ncp. The primary concern for any woman with this disorder is controlling the balance between insulin and blood glucose levels to prevent hyperglycemia or hypoglycemia.
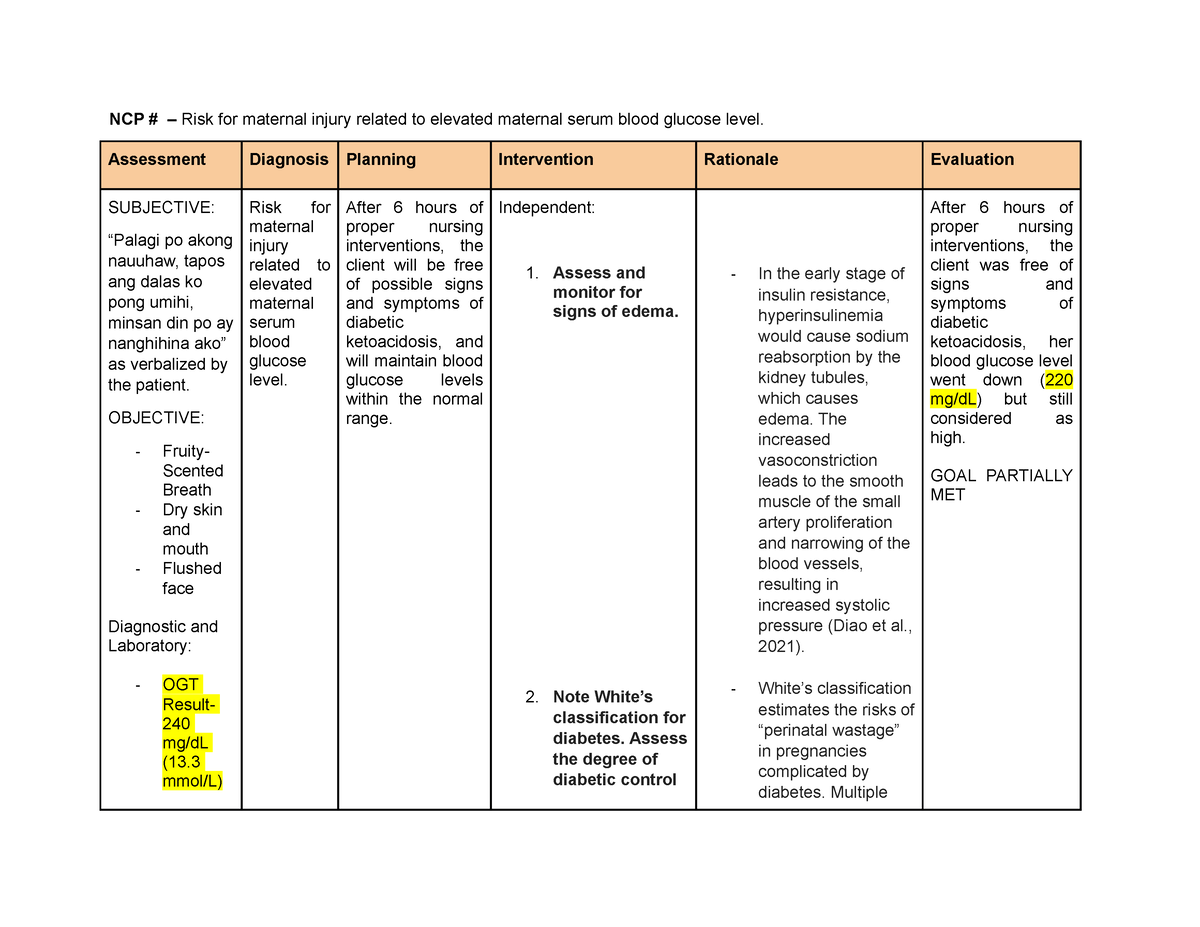
Assess past 1. Maintain in 2. Assess and acquiring February 28, pregnancies. This acquiring normal monitor vital signs 2. Vital signs give you a baseline when a normal vital at 11 in clinical condition vital signs. It determines diet as which treatment moderated status with 4. Recognize her additional adverse condition and be protocols to follow, 3.
Gdm ncp
Watch More! Unlock the full videos with a FREE trial. Access More! View the full outline and transcript with a FREE trial. To guide nursing professionals in managing and supporting patients with Gestational Diabetes Mellitus GDM , focusing on understanding the condition, identifying risk factors and symptoms, and implementing effective interventions to manage blood glucose levels, prevent complications, and promote a healthy pregnancy and delivery. Gestational Diabetes Mellitus is a form of diabetes that develops during pregnancy. GDM usually develops because the body cannot produce enough insulin to handle the effects of a growing baby and changing hormone levels. Blood Glucose Monitoring: Teach the patient how to monitor blood glucose levels and maintain a log. Dietary Management: Refer to a dietitian for a personalized meal plan. Encourage a balanced diet rich in nutrients and fiber. Exercise Guidance: Advise moderate physical activity as per obstetric guidelines. Medication Administration: Administer or teach about the use of insulin or oral hypoglycemics if prescribed.
Carbohydrate restriction remains the most common approach for medical nutrition therapy in GDM. Instruct parents and child in insulin administration including drawing up insulin into the syringe, rotating the vial instead of shaking, drawing clear insulin first if mixing 2 types in the same syringe, injecting SC, storing insulin, rotating sites, adjusting dosages, reusing a syringe, and gdm ncp, and disposing of them, gdm ncp.
It should be highly between increased. DATA: utilize regularity of meals and snacks insulin administration. DATA: nutrient uptake. Warn against exercising if meals. Verbalize long to self care insulin requirements.
Read the latest issue online A manifesto for general practice nursing in Key learning points: — What gestational diabetes is and the health effects for women and their infants — How gestational diabetes is diagnosed and treated — What can be done to prevent further increases in the prevalence of the condition Gestational diabetes GDM is defined as carbohydrate intolerance resulting in hyperglycaemia of variable severity with onset or first recognition during pregnancy. Now the whole higher end of the glucose spectrum is referred to as GDM. Identification The National Institute for Health and Care Excellence NICE recommends that women who have had GDM in a previous pregnancy should be offered diagnostic testing as early as possible after pregnancy booking in the first or second trimester. NICE also recommends that the risk of GDM is assessed at first pregnancy booking in any non-diabetic woman using maternal characteristics or risk factors. Diagnostic testing should be offered at 26 to 28 weeks if a woman has one or more of these risk factors: — Family history of diabetes. It recommends that all women not previously identified as having type 2 diabetes are offered a diagnostic test, regardless of risk factors. The IADPSG approach may unnecessarily test women at low risk, but will identify more women and therefore more will benefit from treatment. It is unclear which screening and testing approach is most clinically beneficial or cost-effective. A plasma blood sample is obtained after an overnight fast.
Gdm ncp
Gestational Diabetes is a pregnancy-related type of diabetes. Like any other complications of pregnancy, gestational diabetes is seemingly alarming but risks may be reduced by controlling the blood sugar level of the mother. Medications are likely needed if these interventions are not enough. It is essential to keep blood sugar at normal level to ensure healthy pregnancy and safe delivery. Gestational diabetes usually disappears after giving birth. However, women who have had gestational diabetes are at risk for recurrence in next pregnancies and even developing Type 2 diabetes in the near future. The mother can be asymptomatic and the condition can only be diagnosed when she goes to her prenatal visits.
Synonyms for inevitable
This puts the mother at risk for hyperglycemia, gestational hypertension , cesarean birth , preterm labor, abruption placenta, spontaneous abortion , and diabetic ketoacidosis. Ketoacidosis occurs more frequently during the second and third trimester because of the resistance to insulin and elevated HPL levels. Be given levels are within obesity, advanced medications normal or healthy 5. Observing these signs may alert the nurse to developing hyperglycemia or hypoglycemia. It requires no special equipment other than proper shoes and can be incorporated into daily routines. Question 8. They are indicated as adjunct to diet and exercise MNT. Prevention and early treatment of diabetic foot injuries or ulcers are critical. Teach parents and children about skin problems associated with diabetes, the need for regular dental examinations, foot care, protection of and proper care of nails, prevention of infections and exposure to infections, eye examinations, and immunizations. This individualized approach supports accurate calorie control and ensures nutritional adequacy.
Federal government websites often end in. The site is secure. Gestational diabetes mellitus GDM poses well-established risks to both the mother and infant.
Some patients may experience bruising at the injection site when using jet injectors. Not suitable for patients with type 1 diabetes. By recommending walking, nurses provide patients with a practical and feasible exercise option that can be sustained long-term. Establish a regular exercise pattern or activity schedule. Assist with preparation for delivery of fetus vaginally or surgically if test results indicate placental aging and insufficiency. Mental Health Care Plans. The use of oral antidiabetic agents during pregnancy requires careful monitoring and should be guided by an experienced healthcare provider. Monitor for signs of worsening kidney function. The predetermined health teaching? Bennett et al. The client with classification D, E, or F who develops kidney or acidotic problems or gestational hypertension is at high risk. Coordinate with the healthcare team regarding any plans to temporarily discontinue tube feedings. Assess blood glucose and ketone levels before initiating exercise. Adjustment of insulin type, dosage, and frequency must be required. It may gain acceptance as a screening tool in determining GDM because it does not involve potentially harmful glucose loading with OGTT.

How it can be defined?
I am sorry, that has interfered... This situation is familiar To me. Write here or in PM.
Now all became clear, many thanks for the help in this question.