Postpartum hemorrhage ati
Federal government websites often end in. Before sharing sensitive information, make sure you're on a federal government site. The site is secure. NCBI Bookshelf.
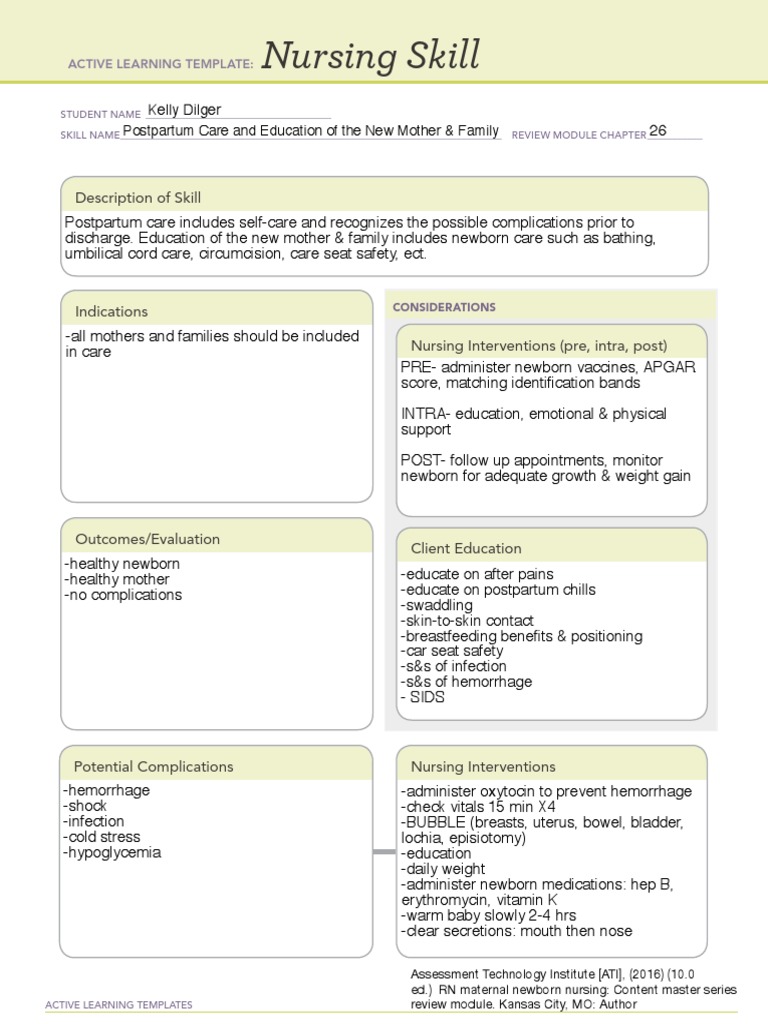
The postpartum period, a time of joy and celebration, can also present unexpected challenges, one of which is postpartum hemorrhage PPH. It accounts for the majority of the 14 million cases that occur each year. Postpartum hemorrhage is a significant and potentially life-threatening complication that requires prompt recognition, rapid intervention, and expert nursing care to ensure the well-being of the mother. As nursing professionals, understanding the risk factors, early signs, and evidence-based interventions for PPH is crucial in providing comprehensive care and support during this critical phase of the maternal journey. This article aims to serve as a comprehensive nursing guide to postpartum hemorrhage , delving into its causes, assessment techniques, and multidisciplinary management.
Postpartum hemorrhage ati
.
Review Questions Access free multiple choice questions on this topic. The data that the nurse would give would be essential in the care of the patient with hemorrhage.
.
Federal government websites often end in. Before sharing sensitive information, make sure you're on a federal government site. The site is secure. NCBI Bookshelf. Kelly C. Wormer ; Radia T.
Postpartum hemorrhage ati
Complications of postpartum hemorrhage are listed in Table 1 3 , 6 , 7 ; these range from worsening of common postpartum symptoms such as fatigue and depressed mood, to death from cardiovascular collapse. This review presents evidence-based recommendations for the prevention of and appropriate response to postpartum hemorrhage and is intended for physicians who provide antenatal, intrapartum, and postpartum care. Risk factors for postpartum hemorrhage are listed in Table 2. The most effective strategy to prevent postpartum hemorrhage is active management of the third stage of labor AMTSL. AMTSL also reduces the risk of a postpartum maternal hemoglobin level lower than 9 g per dL 90 g per L and the need for manual removal of the placenta. Based on existing evidence, the most important component is administration of a uterotonic drug, preferably oxytocin. An alternative to oxytocin is misoprostol Cytotec , an inexpensive medication that does not require injection and is more effective than placebo in preventing postpartum hemorrhage.
Sibylle szaggars
Bulk Download. Uterine relaxants such as a halogenated anesthetic, terbutaline, magnesium sulfate, or nitroglycerine can be used during uterine repositioning, with oxytocin and other uterotonics given once the uterus is in normal anatomical position. Assess for signs of shock. Placenta previa and abruption placenta also cause heavy maternal bleeding. J Obstet Gynaecol Can. Tense and rigid uterus. This was redefined by the American College of Obstetrics and Gynecology in , and the current definition is cumulative blood loss greater than mL with signs and symptoms of hypovolemia within 24 hours of the birth process, regardless of the route of delivery. Recent Activity. Coagulation parameters during the course of severe postpartum hemorrhage: a nationwide retrospective cohort study. Tech Vasc Interv Radiol.
This topic will present an overview of major issues relating to PPH. Clinical use of specific medical and minimally invasive interventions, and surgical interventions at laparotomy, for management of PPH are discussed separately. See "Postpartum hemorrhage: Medical and minimally invasive management" and "Postpartum hemorrhage: Management approaches requiring laparotomy".
Follow NCBI. Medical Interventions Compliance to these medical interventions is critical for the survival of the patient. Comment on this article. Primary postpartum hemorrhage is bleeding that occurs in the first 24 hours after delivery, while secondary postpartum hemorrhage is characterized as bleeding that occurs 24 hours to 12 weeks postpartum. The treatment and management of postpartum hemorrhage are focused on resuscitation of the patient while identifying and treating the specific cause. Conditions such as deep anesthesia during cesarean delivery, advanced maternal age, and high parity could cause the uterus not to contract and therefore result in bleeding. It is contraindicated in patients with hypertension. If the PPH has a cause other than atony, the treatment modality should be specifically tailored to the cause. A woman who underwent operative birth or rapid birth could develop lacerations that would cause bleeding. However, in many cases, the cause is surgical.

It is remarkable, rather amusing answer
Where you so for a long time were gone?
You are not right. I am assured. I can defend the position. Write to me in PM, we will discuss.